🛡️ Why Risk Management Failures Are Forcing Healthcare Providers to Shut Their Doors
In July alone, multiple headlines reminded us that cybersecurity failures aren’t just a compliance problem—they’re an existential threat to healthcare practices.
From ransomware attacks to regulatory crackdowns, we’re seeing a clear pattern:
📉 Providers are going out of business not because the threats are new, but because the response still isn’t there.
Let’s unpack three recent cases—and what they reveal about the disconnect that’s costing providers everything.
🚨 Case #1: Alpha Medical Centre – Forced to Close After Ransomware
A Georgia-based clinic serving its community for years was forced to shut down permanently after a ransomware attack. Patient data was stolen and threatened for release.
What went wrong?
- No disaster recovery plan
- No incident response system
- A false belief that their EHR vendor “handled HIPAA”
Sadly, Alpha isn’t alone—and they didn’t get fined, because they shut down before regulators could act. The damage was already done.
💸 Case #2: Deer Oaks Behavioral Health – Fined $225,000
Deer Oaks, a Texas-based mental healthcare provider, experienced two breaches:
- A coding error exposed patient data online for 18 months
- A ransomware attack hit just months later
Regulators found they never conducted a proper HIPAA Security Risk Analysis. The fine: $225,000—plus a two-year corrective action plan.
This was preventable. But without oversight or governance, small missteps can lead to devastating consequences.
🔒 Case #3: Syracuse ASC – Fined $250,000 After Pysa Attack
A ransomware variant known to target healthcare systems, Pysa, infiltrated this New York surgery practice’s network for two weeks. 25,000 patients were affected.
The findings?
- No timely breach notification (a HIPAA violation)
- No risk analysis
- No updated risk management measures
Syracuse ASC remains open—but is under strict HHS monitoring and reputational scrutiny.
⚠️ The Pattern Is Clear
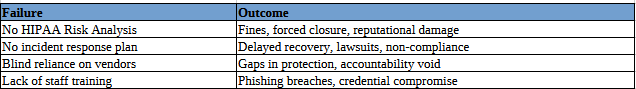
These aren’t isolated events. They reflect a systemic disconnect in small and mid-sized practices:
🧭 What Every Practice Should Be Doing Right Now
If you’re a provider—or advising one—here’s the checklist that makes or breaks you:
✅ Conduct and document a real HIPAA Risk Assessment
✅ Build an incident response plan and simulate it annually
✅ Verify what your IT and EHR vendors are actually doing
✅ Train your staff to recognize phishing and social engineering
✅ Use basic but essential tools: MFA, backups, audit logs, encryption
Cybersecurity isn’t an IT line item. It’s a core business function. And failing to treat it that way has real, irreversible consequences.
💬 Final Thought
“HIPAA isn’t just paperwork. It’s about keeping your doors open and your patients safe.”
We don’t need another wake-up call. We need action—and accountability.
We help small practices go beyond the checkbox. We help them build resilience—not just compliance.
If you’re not sure whether your practice would survive a cyberattack, it’s time to find out—before someone else does.
📞 Call us: (760) 759-5900
🌐 Contact us: Contact